What is a retinal tear?
The eye is like a camera with the lenses at the front and the photographic film (retina) at the back. Between the two in the “body” of the camera is a clear jelly called vitreous. This jelly gradually degenerates with the passage of time into a more watery consistency and eventually when sufficient water has accumulated in the jelly the remaining jelly that is up against the retina separates from it and in most people collapses down into smaller lumps causing some floaters in the vision which usually improve as they float down to the bottom of the eye with gravity.
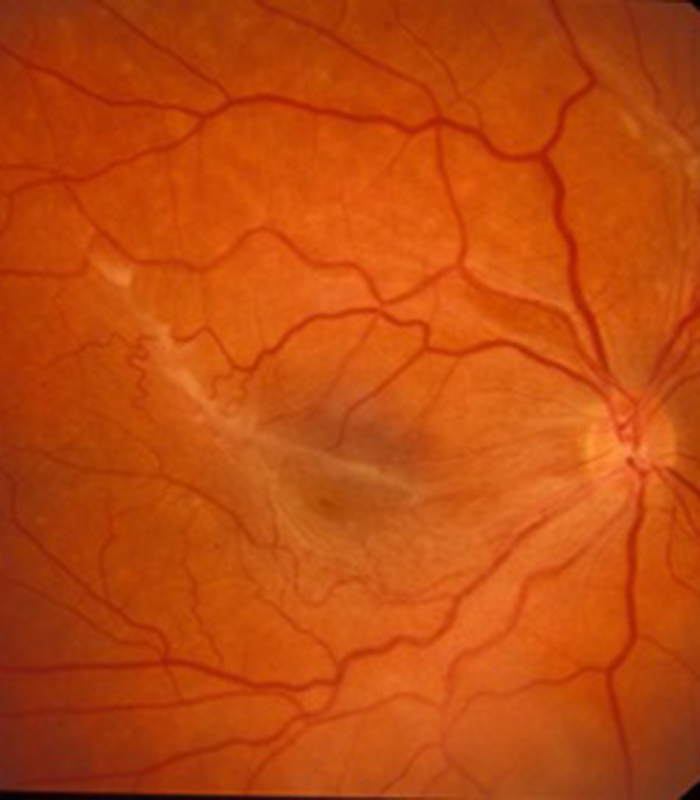
A small number of patients however have abnormal adhesion or stickiness between the remaining jelly and the retina in places and as the jelly pulls away it does not want to “let go” of the retina in this position and pulls sufficiently hard to tears the retina. These patients usually notice a sudden shower of new floaters associated with flashing light sensations as the retina tears. Patients who are short sighted are more prone to this occurring as their jelly degenerates at a younger age that normal sighted people and they are also more likely to have abnormal adhesion between the retina and jelly. If a retinal tear is diagnosed quickly then treatment can be applied as an out-patients procedure to “spot weld” it in place with laser.
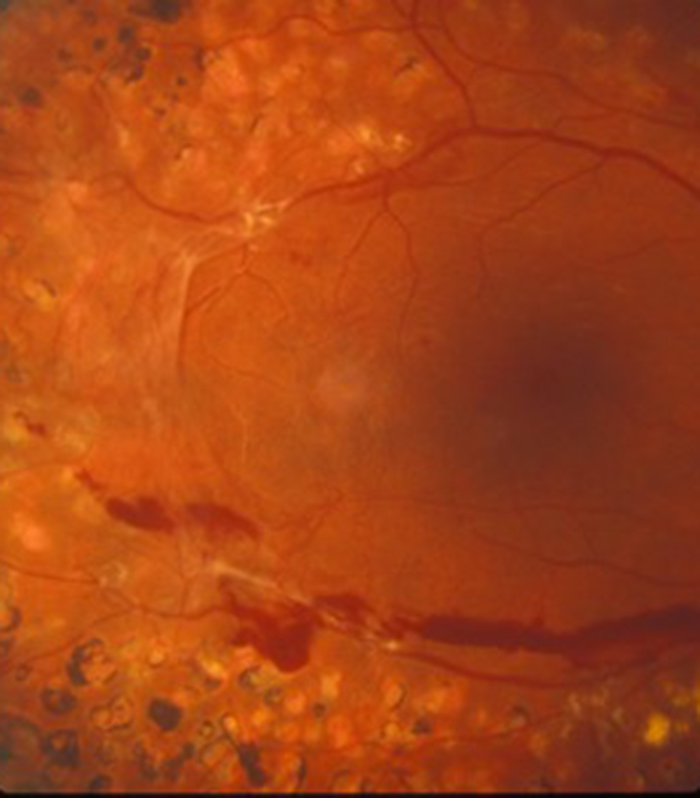
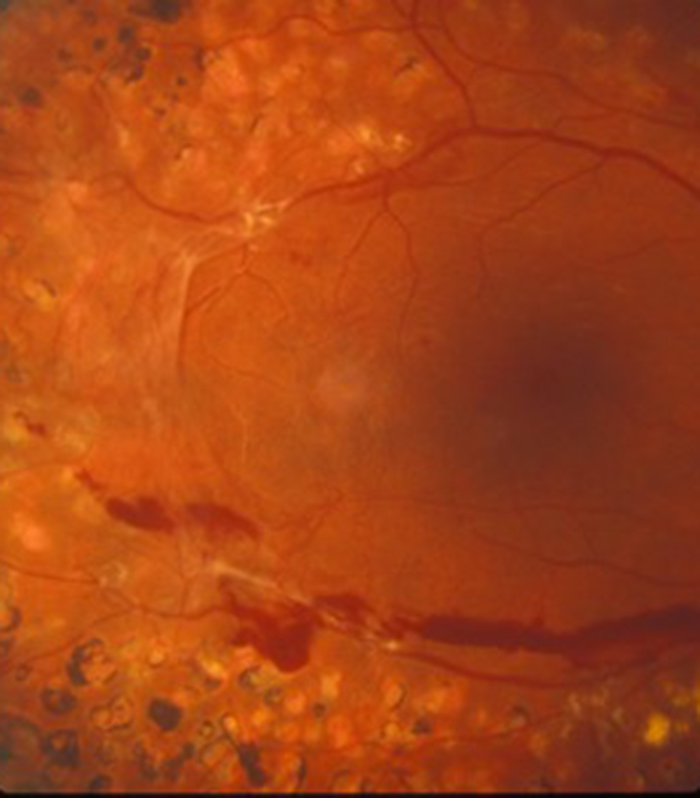
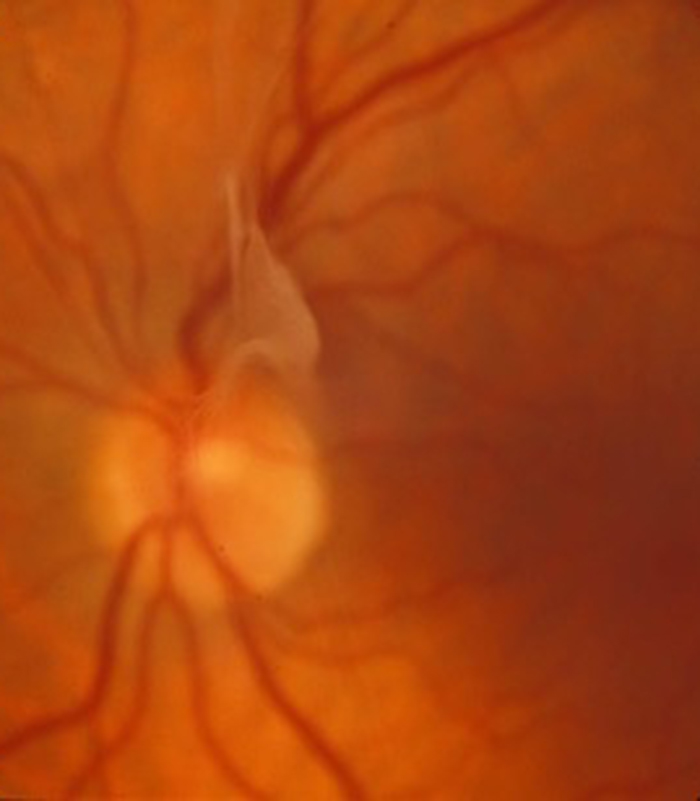
If left untreated the tear in the retina usually progresses into a retinal detachment as the watery component of the jelly in the main eye cavity can get underneath the retina through the tear and the retina starts to come away from the back wall of the eye. When the retina starts “detaching” from the back wall of the eye it comes away from its main blood supply and therefore stops functioning and the detached retina results in a blurred patch in the vision. The blurring usually therefore comes on after a sudden onset of flashes and floaters and develops over hours or days as a dark shadow you cannot see through and appears initially from the side or periphery of the vision and as the detachment spreads towards the centre of the retina (macula) so the blurred patch increases towards the centre of the vision. If left untreated the whole retina can detach results in very poor vision.
It is best therefore to treat the retinal tear before the retina detaches with laser but if the retina starts to detach it is still important to treat as soon as possible as the prognosis for obtaining good vision following surgery if much better if caught at an early stage and in particular if surgery takes place before the central retina (macula) detaches.
What is the surgical treatment of retinal detachment?
Most retinal detachments occur when the jelly (vitreous) that occupies the main eye cavity starts to liquefy and pulls away from the back of the eye but does not want to “let go” of a particular area of the retina (photographic film lining the back wall of the eye). The retina tears in this location and the watery component of the jelly (the part that has liquefied) can pass thought the tear under the retina and the retina starts coming away (detaching) from the back wall of the eye. If left untreated the retina completely detaches and the vision is lost in that eye.
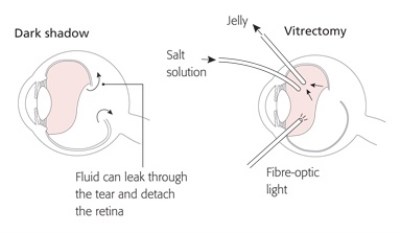
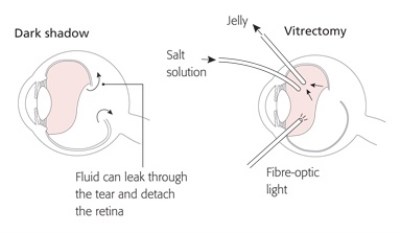
Once the pulling force that caused the tear has been removed, a pushing force is needed to push the retina back into place up against the back wall of the eye and up against one of its blood supplies called the choroid. The retina is too delicate to be physically pushed by instruments and therefore a gas bubble is used and placed into the eye cavity and it is the gas bubble that pneumatically pushes the retina up against the back wall of the eye and into its normal position. Once the retina is in its normal position the tear (or tears) that resulted in the original problem need to be sealed to stop the retina from re-detaching. This is performed by applying laser around the tear(s) to “spot weld” them in place. The laser treatment does not however have an immediate effect as it works by creating inflammation in the retina and it is only when this inflammation changes into scar tissue that the full seal develops.
The retina therefore needs to be held in the correct position whilst this scarring is taking place and hence the need to “posture” following retinal detachment surgery. The posturing allows the gas bubble to float up against the tear and keep it pressed against the back wall of the eye whilst the scarring develops. The position of the posture depends on where the tear or tears are situated. The duration of the posturing also depends on the size and position of the tear(s) and the type of gas used. It is rare that posturing is needed for more than a week and is usually between 3 to 5 days. During this time however it does require a commitment from the patient to keep in position and this can be very difficult and does need help. I normally suggest that the posture needs to be adopted for 50 minutes in every hour so that 10 minutes is available for stretching the legs, going to the loo and having something to eat. There are various posturing aids available and are usually lent to patients from the day case ward where they have surgery. The face down posture is the most difficult one to adopt. At night it is impossible to posture face down so I suggest lying on your stomach and alternating your left and right cheek to the pillow. Your surgeon should however give you specific instructions on the exact posturing requirements for you eye as every retinal detachment is different with respect to the position, size and type of tears therefore the posturing regimen has to be tailored to your particular retinal detachment.
Whilst the gas is inside the eye the vision will be very blurred and then it will gradually improve as the gas gets absorbed back into the blood stream. Different gases are used depending on the type of detachment and the gas can last anywhere between 1 week if air is used to 6 weeks with a long acting gas. It is advisable not to drive until the gas bubble has completely disappeared and you must certainly not fly or go up at altitude such as a high mountain. If you have a general anaesthetic for any other condition whilst there is still some gas in the eye then do please ensure that the anaesthetist knows about your gas bubble as again some gases can cause the pressure to increase in the eye. You should have a wrist band stating that you have a gas bubble after the operation and this should only be removed once the gas bubble has completely disappeared. When the eye is full of gas immediately after surgery the vision will be very poor but this is to be expected as the gas does not allow the light to focus very well. Sometimes however if you adopt a face down position and then put something very close to your eye such as a wrist watch, you may get a vague focus as usually eyes become optically short sighted when the eye ie full of gas. As the gas slowly gets absorbed into the blood stream it gets replaced by a clear fluid called aqueous humour which is produced at the front of the eye and usually stays at the front of the eye. After a vitrectomy and gas procedure however for retinal detachment, as the gas disappears it gets replaced in the main eye cavity (vitreous cavity) by the aqueous. Inside the eye the gas is shrinking upwards (due to its buoyant nature) but you perceive the opposite effect as things are optically reversed by the eye. You initially see some clarity of vision as a crescent at the top of your vision and this then slowly moves down as if the bubble is sinking to the bottom of the eye.
Usually after about 2 to 3 weeks you become a human “spirit level” with half and half split vision with a clear area in the top half of the vision and a wobbly blurred area in the lower half of the vision. Often when the bubble gets very small it breaks up into small bubbles due to changes in surface tension of the bubble before it completely disappears. You will be able to tell the exact day the bubble has gone!
If the central retina (macular) has detached for any length of time prior to surgery the central vision may not return completely even with successful reattachment of the retina. This is why it is so important to treat the condition as quickly as possible. The retina can be successfully reattached nine times out of ten with one operation but sometimes further surgery is needed. If excess scar tissue forms inside the eye (not related to the laser) it can contract and pull the retina off once more. If this occurs more extensive surgery is required to remove the scar tissues and sometimes clear silicone oil has to be placed in the main eye cavity to keep the retina in position for several months before the oil is removed with another operation. New holes can develop in the retina after surgery or old holes can reopen and this is also a cause for the retina re-detaching.
Sometimes holes develop in the retina due to gradual thinning of the retina rather than the jelly pulling on the retina. These are called atrophic holes and are less frequently seen but may be treated in a different way. These holes can be sealed from the outside rather than the inside and this usually involves placing some plastic called a scleral buckle on the outside of the eye overlying where the hole is situated. The buckle is stitched to the sclera (the white of the eye) and this creates an indentation pushing the sclera in towards the hole in the retina and this helps seal the tear. The buckle stays in position permanently but is covered by the conjunctiva which is the skin that covers the white of the eye and is therefore not visible. A scleral buckling procedure usually does not require gas inside the eye or any posturing. These sorts of atrophic holes tend to cause retinal detachments in younger patients. There is also another type of tear in the retina called a retinal dialysis where tends to occur in younger patients and also is seen following blunt trauma to the eye which requires surgery with a plastic buckle from outside the eye rather than vitrectomy surgery.
The manipulation to the eye required for buckling procedures is greater that the 3 small holes that are only needed for vitrectomy surgery so the eye can be a little more uncomfortable after buckling than vitrectomy. The vast majority of patients needing surgery for retinal detachment are due to the vitreous jelly tearing a hole in the retina and need treatment with vitrectomy surgery. The operation is sometimes called a “3 port pars plana vitrectomy” as the surgery is performed though 3 small incisions towards the front of the eye in the sclera or “white of the eye”.
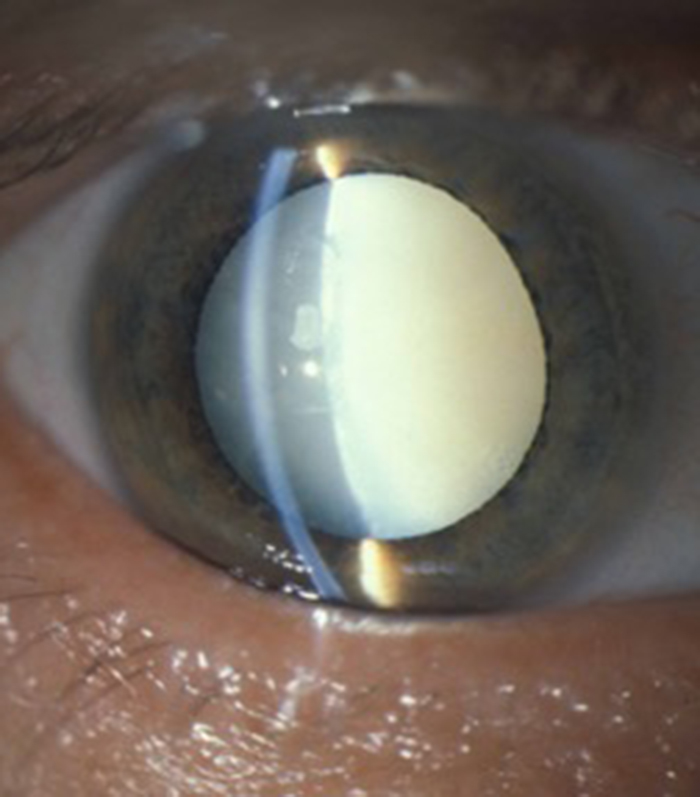
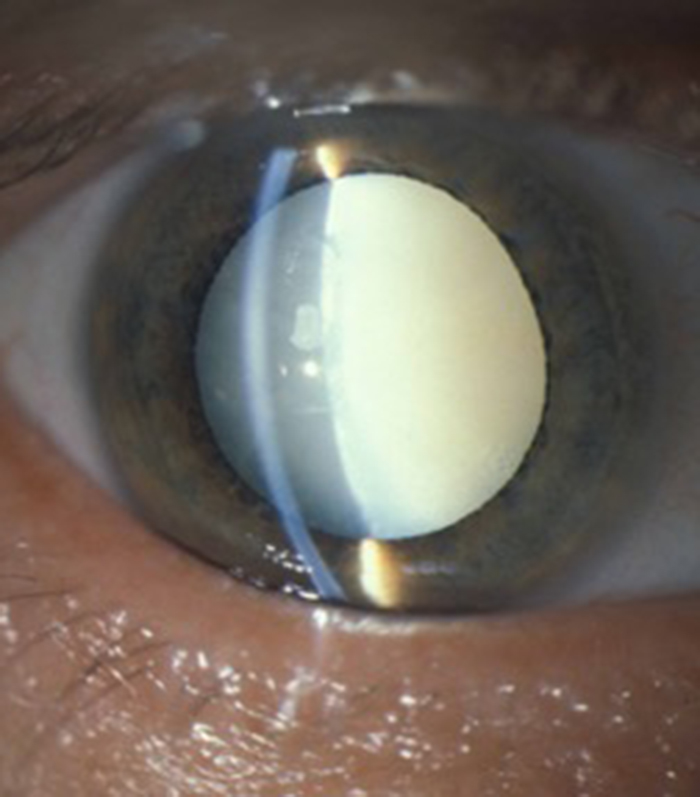
The size of instruments and therefore the size of holes created is getting smaller and smaller and I routinely perform surgery with either 23 gauge or more frequently 25 gauge vitrectomy instruments depending on the individual case. Most of the holes in the white of the eye (called sclerostomies) are self sealing but sometimes fine self dissolving stitches are required to ensure the hole has fully closed. The eye can feel a little gritty after vitrectomy surgery but it should not be painful and usually Paracetamol is all that is needed in the first couple of days after surgery together with taking drops, usually 4 times a day but sometimes more frequently if extensive surgery is required. Vitrectomy surgery usually causes cataract to form or progression of cataract if it is already present. It is therefore likely that cataract will develop usually many months but sometimes years after cataract surgery. A cataract is a cloudy lens inside the eye and there are two main types of cataract associated with vitrectomy surgery. There is an immediate cataract called a “gas cataract” that is seen straight away after surgery and is due to the gas pressing up against the back of the crystalline lens inside the eye. This often is partially or completely reversible as the gas reabsorbs. There is however another type of cataract called “nuclear sclerotic” cataract which is the classic cataract that gradually develops after vitrectomy surgery. The crystalline lens becomes brown and hard (sclerotic) in its central portion (nuclear) and the vision gradually blurs. For optical reasons patients with this type of cataract often become short-sighted as it develops and become aware that they can see things for near without their reading glasses before the vision blurs at all distances. This lens also has a brown hue and patients may notice a brown or sepia colour to the things they view with the affected eye. In the early stages vision can be improved with a change of glasses but this is only a temporary measure as the cataract progresses. If there is sufficient cataract to cause problems surgery is indicated. Most patients having vitrectomy for retinal detachment with therefore need a cataract operation at a later date if they have not already had cataract surgery prior to their developing a retinal detachment. If at the time of retinal detachment the view to the back of the eye is so poor due to pre-existing cataract then “combined surgery” is performed with the cataract being removed at the same time. My experience however is that in most situations it is better to get the retinal successfully reattached in the first instant and then tackle the cataract with a second operation at a later date. Retinal detachment surgery is usually performed under local anaesthetic with some sedation but can be performed under general anaesthetic (with the patient fully asleep) if the patient is anxious or if extensive surgery is required that may take some time. It is performed as a day case procedure and there is not need for patients to stay in hospital overnight. Most detachment operations take in the region of 45 minutes to 90 minutes. The cataract operation that is needed some time after the detachment repair is usually a 20 minute procedure.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
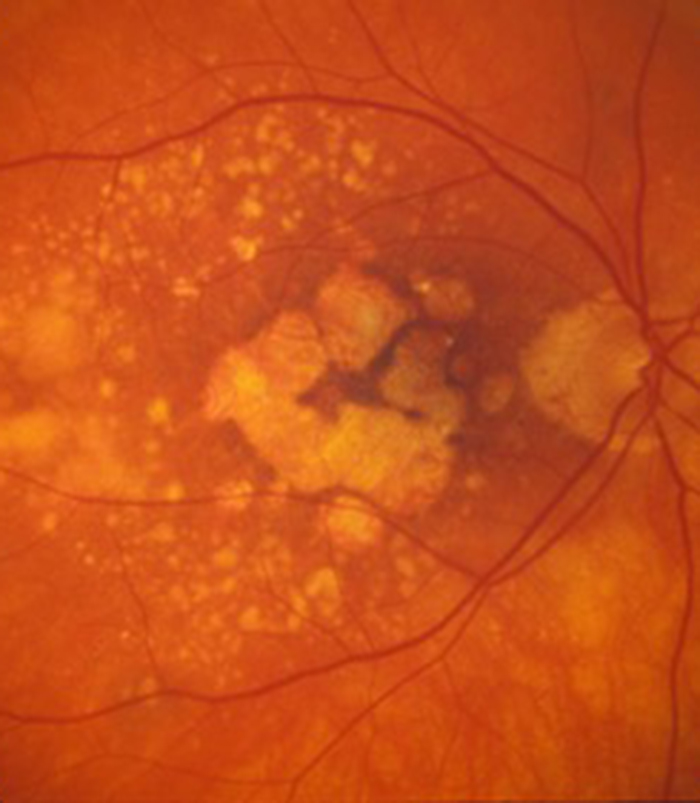
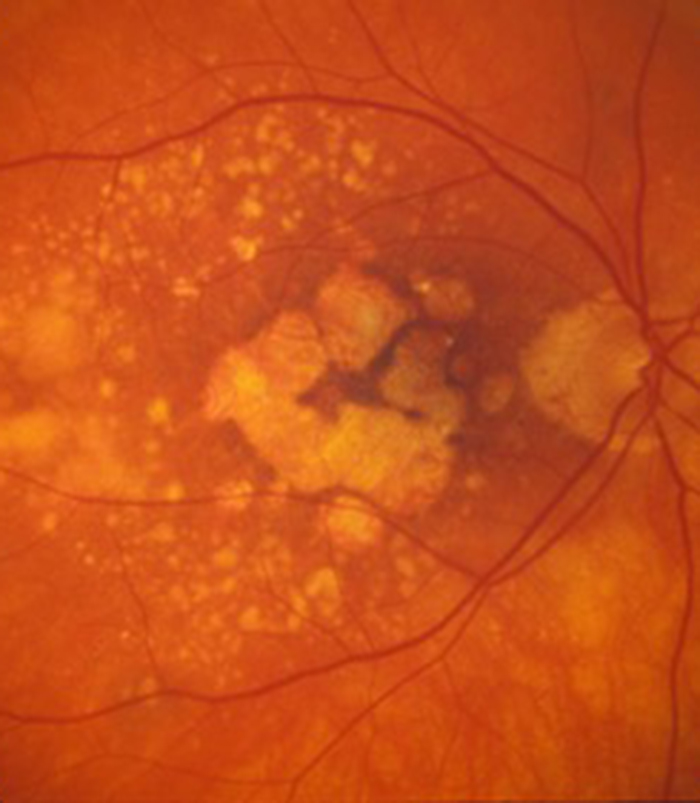
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
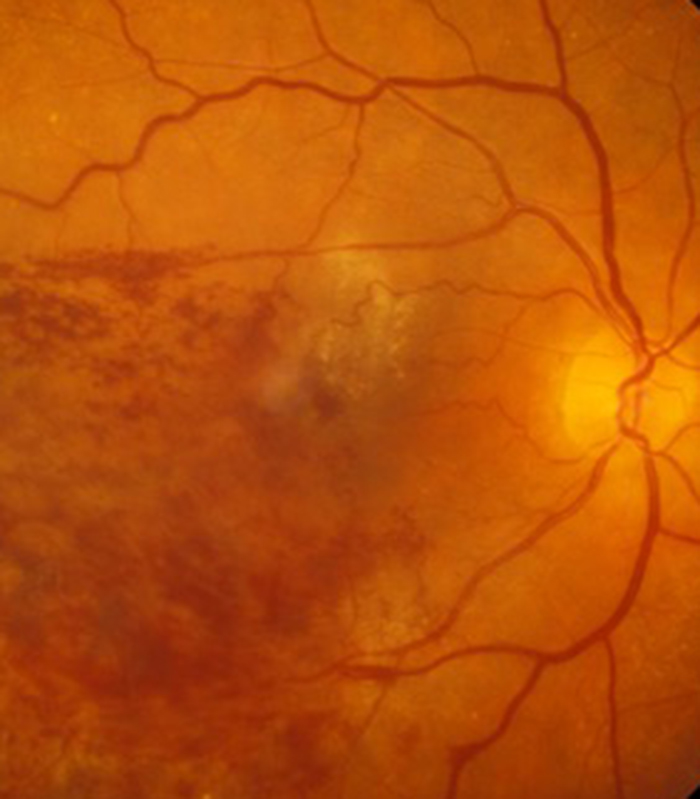
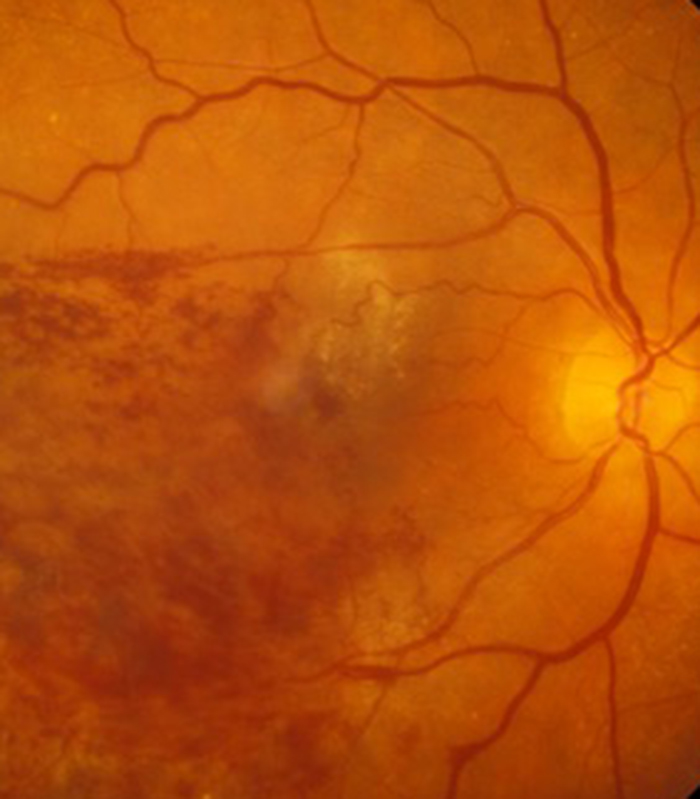
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
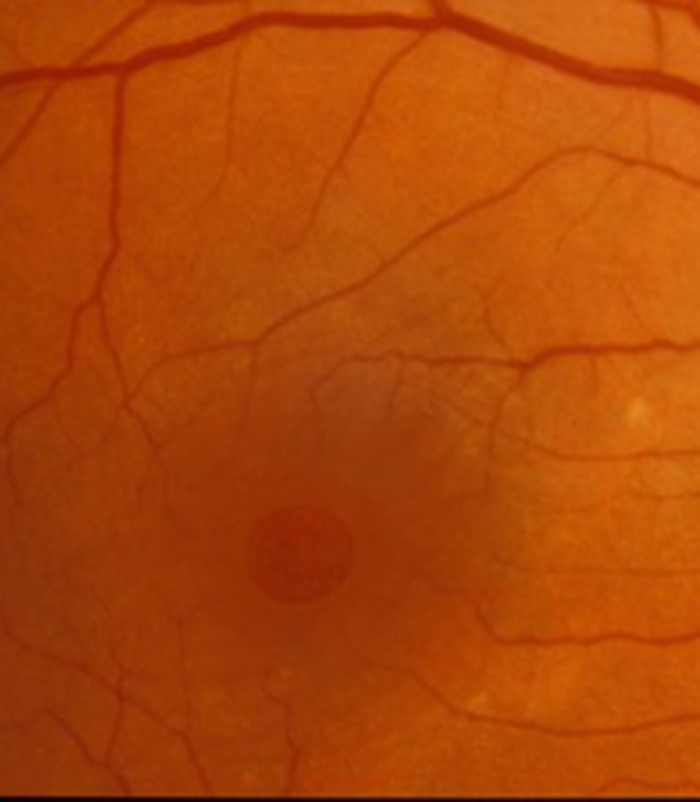
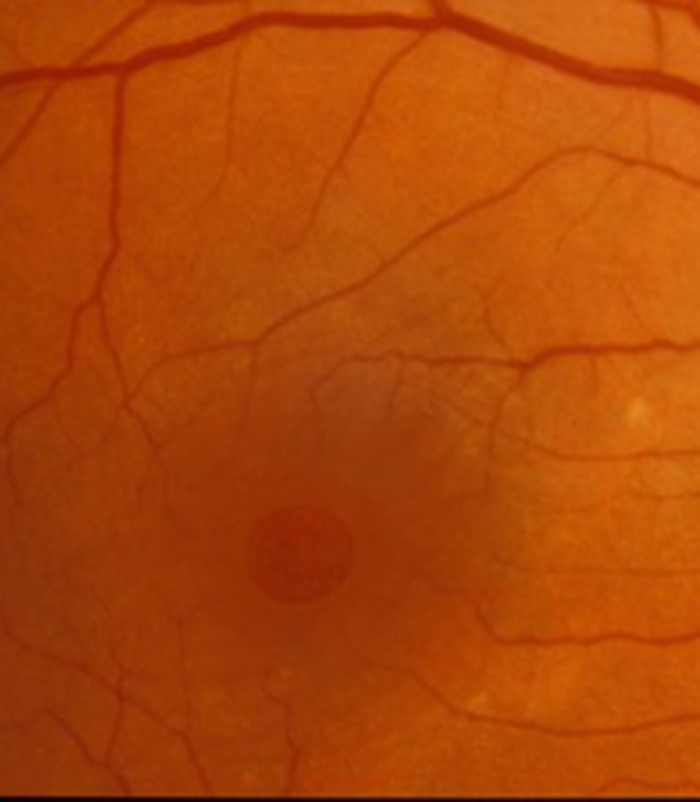
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.
Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

