What is an epiretinal membrane?
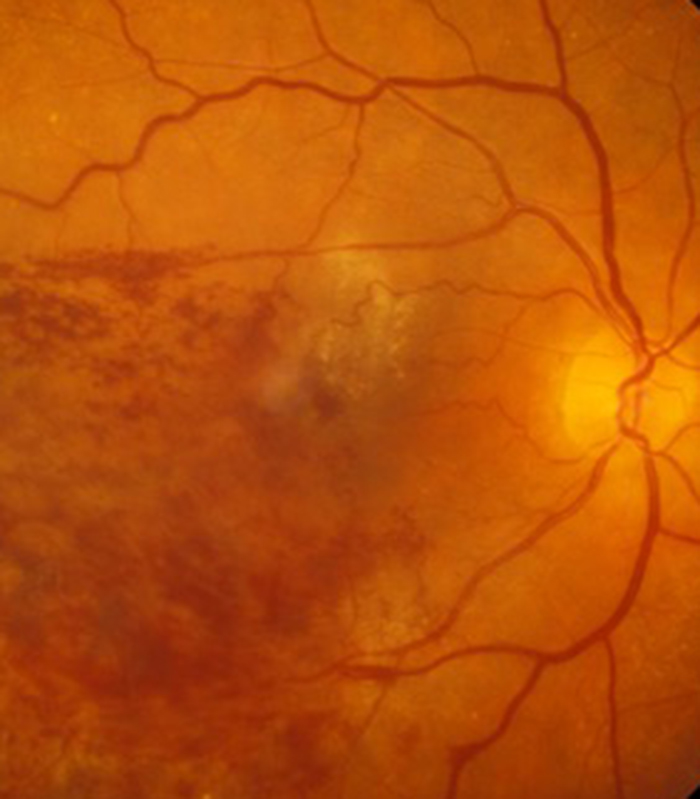
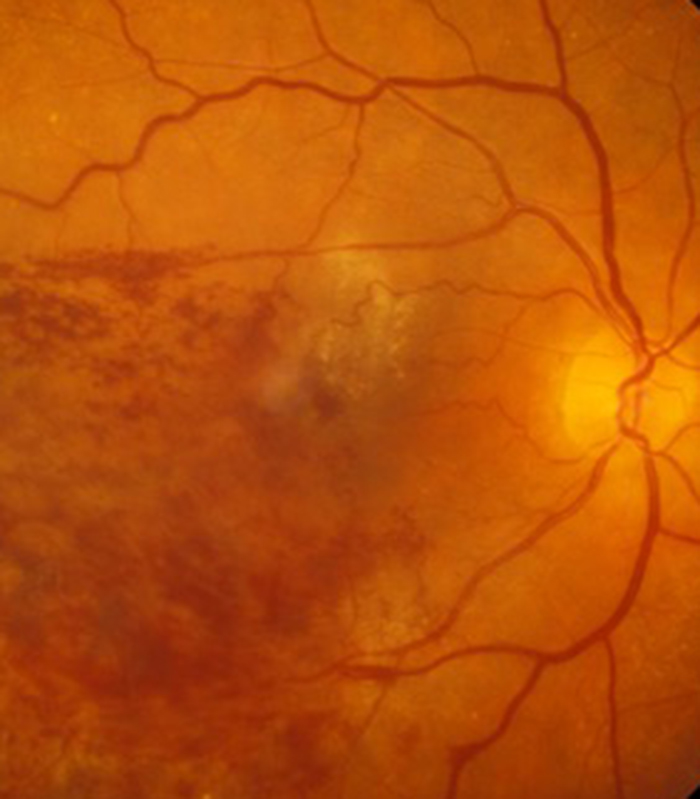
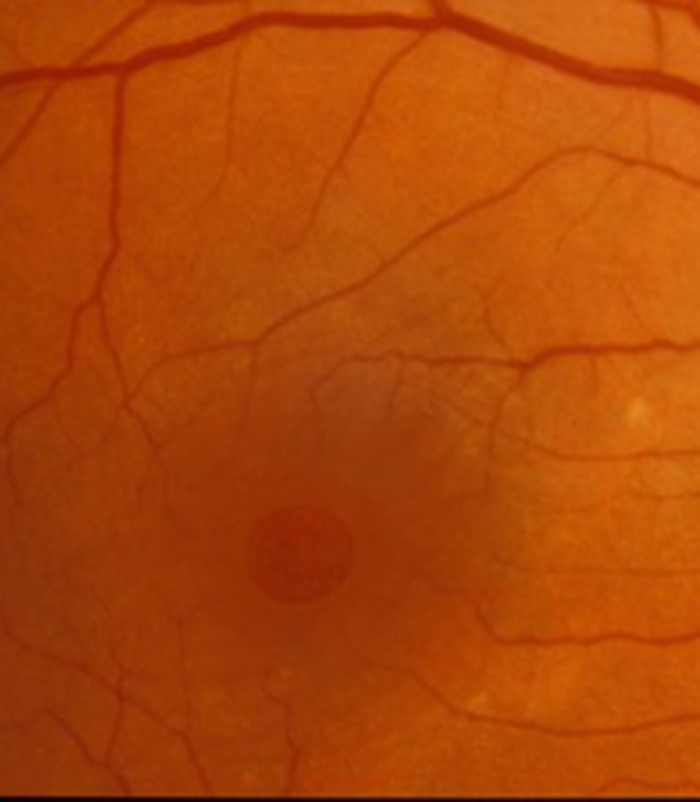
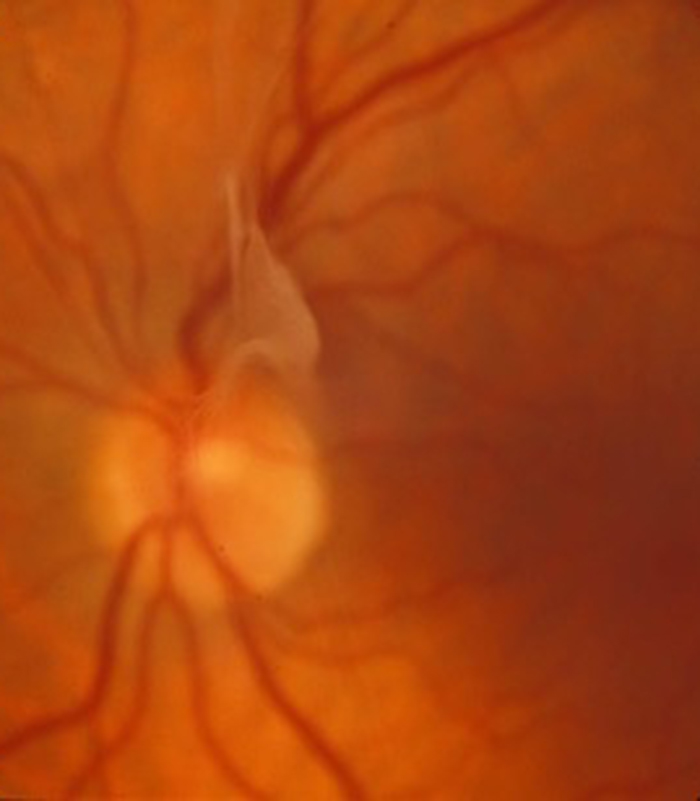
Some patients develop a thin layer of scar tissue on the surface of the centre of the retina (macula) called an epiretinal membrane (sometimes also called cellophane maculopathy). This thin layer of scar tissue does two things, it impairs the light getting to the retina (causing blurring of central vision) and it contracts (causing wrinkling of the underlying retina with distortion of vision).
Scar tissue formation is often associated with a degenerative change within the jelly that occupies the main eye cavity. The jelly is called vitreous and with the passage of time it turns from being a jelly like substance to a more watery consistency. This watery consistency allows cells (including scar tissue cells) to move around more freely inside the eye and the scar tissue cells like to settle on the macula where they form a sheet of tissue attached to the retina. The main reason we have evolved to develop scar tissue is to help with wound healing as scar tissue likes to contract to pull the edges of a wound together. This is helpful if you have a cut to the skin but if a sheet of scar tissue on the surface of the retina contracts it causes the underlying retina to wrinkle. This “bump” that develops on the surface of the retina also results in a “bump” in your vision and hence distortion of vision is a feature of epiretinal membrane formation. The treatment for this condition is a surgical procedure called a vitrectomy and membrane peel to remove the scar tissue from the surface of the retina.
What is the surgical treatment of epiretinal membrane?
Scar tissue can form on the surface of the retina and in particular likes to form at the centre of the retina or macula. This results in a gradual blurring of vision and is often accompanied by distortion of vision as the scar tissue contracts and wrinkles the underlying retina.
The scar tissue can be removed with an operation called a vitrectomy and membrane peel. In order to gain access to the scar tissue on the surface of the retina the jelly (vitreous) that occupies the main eye cavity has to be removed. The surgery is usually performed under local anaesthesia with sedation but can also be performed under general anaesthetic both as a day case procedure. It involves creating three very small incisions in the sclera (white of the eye) at the front of the eye and all instruments are placed through these small incisions (it is called a 3 port pars plana vitrectomy. The vitreous is removed by a small instrument that has a fine guillotine at its tip which sucks up a small amount of the vitreous, cuts it, then the small piece of cut vitreous is sucked up a tube and out of the eye. The cutting edge of the guillotine moves backward and forward many time a second. You may hear a “buzzing” sound at the time of surgery and this is the fine guillotine working inside your eye carefully removing the vitreous piece by piece! As the vitreous is being slowly and carefully removed a saline (salt) infusion is going into the eye to keep it “pumped up” and stop it from collapsing. When the vitreous has been removed the eye initially contains this salt solution and then this is then gradually replaced by a clear fluid called aqueous which is produced by the eye. The aqueous is formed at the front of the eye and usually circulates just at the front of the eye. After a vitrectomy this aqueous occupies the whole eye and the eye functions very well without the vitreous (you will also notice less floaters once the vitreous jelly has been replaced by the watery aqueous). Once the vitreous has been removed a fine pair of forceps is introduced into the vitreous cavity through the small incision at the front of the eye to peel away the scar tissue. In most patients the tissue comes away with ease but sometimes the scar tissue can be “stuck” to the retina and comes away in a piecemeal fashion. This type of surgery on the retina is therefore by its nature not as predictable as cataract surgery where up to 99% of patients will get an excellent result. Most patients having surgery for epiretinal membrane will notice an improvement in their vision and a reduction in the amount of distortion. There may however still be some mild visual disturbance even after technically successful surgery. Things can however continue to improve many months after surgery although most of the improvement tends to occur within the first 3 months.
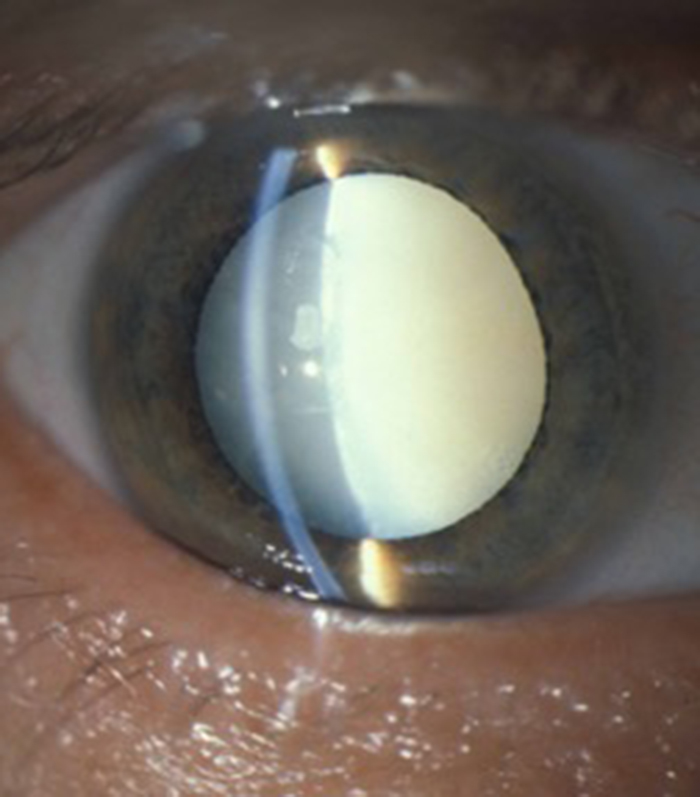
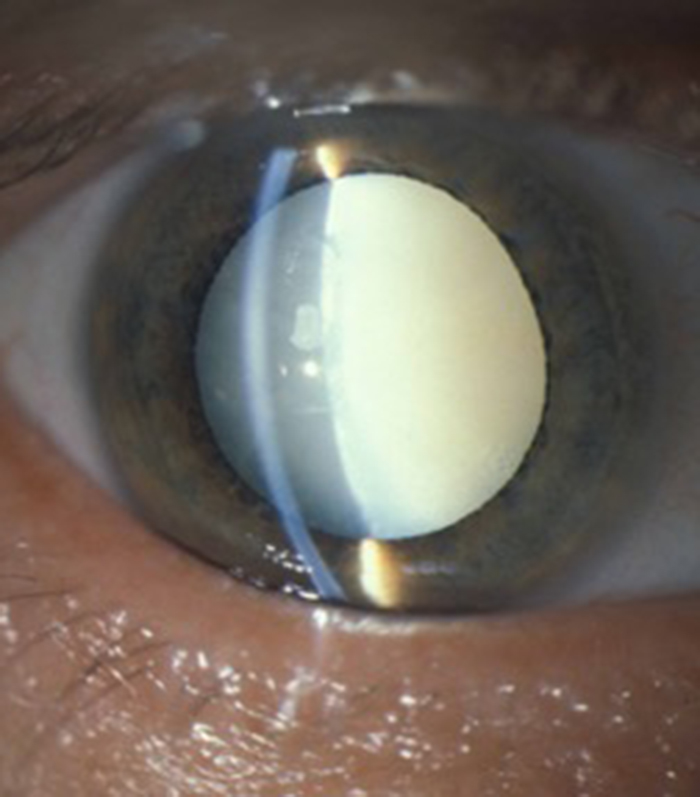
The vitrectomy operation if performed alone will eventually result in the development of a cataract. In patients with mild by symptomatic epiretinal membrane I often perform what is called “combined surgery” for patients. This involves removing the lens of the eye at the time of the vitrectomy surgery and replacing it with a new plastic intraocular lens. This is identical to the cataract surgery which occurs when the lens is cloudy. The advantage of this “combined” approach is that it prevents you having to come back for further cataract surgery months or years after the vitrectomy operation. If however you have a thick and more severe epiretinal membrane I prefer a “two stage” technique where the epiretinal membrane is dealt with in the first instant, the eye is allowed to settle down and then the cataract is operated upon at a later stage once it has developed sufficiently to interfere with the vision. There are two reason for doing a “two stage” technique in more severe epiretinal membranes. Firstly, the combined approach requires a slightly greater degree of manipulation of the eye surgically and this inevitably results in a slightly greater degree of post-operative inflammation. Scar tissue can follow on from inflammation and if an eye is already prone to significant scar tissue forming at the back of the eye there may be a slightly greater risk of recurrence of scar tissue following its removal. By minimising the post operative inflammation (by not performing a combined procedure) following surgery it may reduce the risk of further scar tissue forming on the retina. The second reason for not performing a combined approach with significant epiretinal membrane relates to the way measurements are performed on the eye to calculate the strength of intra-ocular lens implant required for your particular eye at the time of cataract surgery or clear lens extraction (prior to cataract formation). The two main measurements are the curvature of the cornea (clear windows at the front of the eye) and the measurement of the length of the eye from front to back called the axial length. This is the measurement from the front of the cornea to the retina at the back of the eye and is a very critical measurement. Scar tissue as already stated can pull on the retina and cause it to wrinkle and this can make the retina thicken. This can alter the distance from the cornea to the retina. The accurate measurement for cataract surgery is the distance between the front and back of the eye once the scar tissue has been removed and the retinal flattened. The difference in length is small but can have a significant influence on the correct calculation of intra-ocular lens power inserted at the time of cataract surgery. This is why I only perform “combined surgery” on patients with mild epiretinal membrane.
The surgery is performed with small incision microsurgical vitrectomy techniques with either 23 gauge or 25 gauge instrumentation. Sometimes fine stitches are required to to ensure complete wound closure but they are dissolving and do not need to be removed at a later date. The eye can feel a bit gritty after surgery but it should not be painful. Drops need to be instilled usually only 4 times a day for a month to 6 weeks and the vision should gradually improve with also a reduction in distortion.
Any vitrectomy operation including vitrectomy for epiretinal membrane carries the risk of retinal tear formation during removal of the vitreous. If this were to occur then laser is needed during the operation to seal the tear and prevent detachment formation. If a tear does develop then a gas bubble needs to be placed in the main eye cavity and you made need to posture for up to 5 days in a particular position to ensure the tear is sealed properly. The also does mean the vision immediately after surgery is poor until the gas bubble gets absorbed into the blood stream usually 1 to 6 weeks after surgery depending on the gas that needs to be used which depends on the size and location of the tear that develops. It also does mean that you cannot fly or drive until the bubble disappears. There is only a 1 in 10 chance that laser, a bubble and posturing are needed by if you are contemplating this form of surgery it is sensible to keep you diary clear for 6 weeks following the date of your surgery just in case!
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
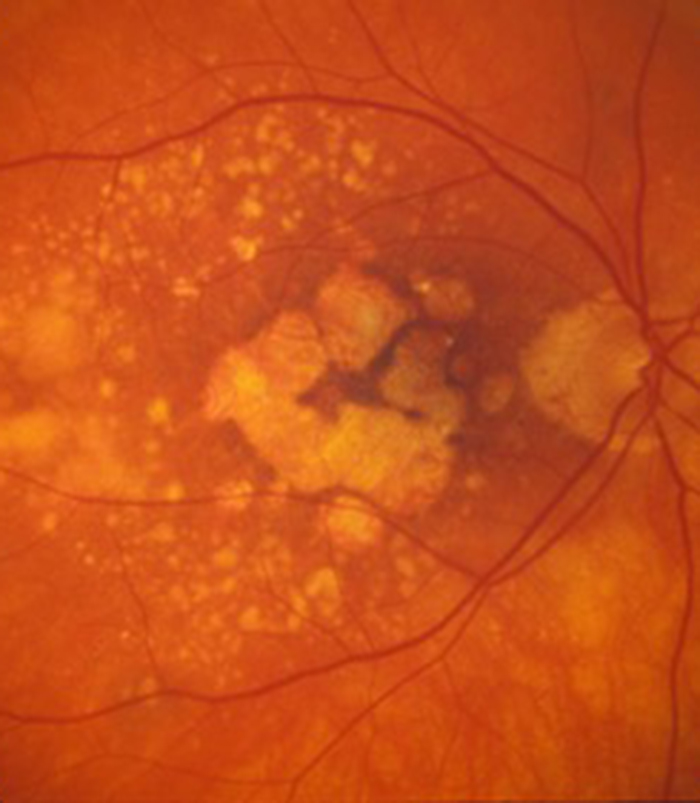
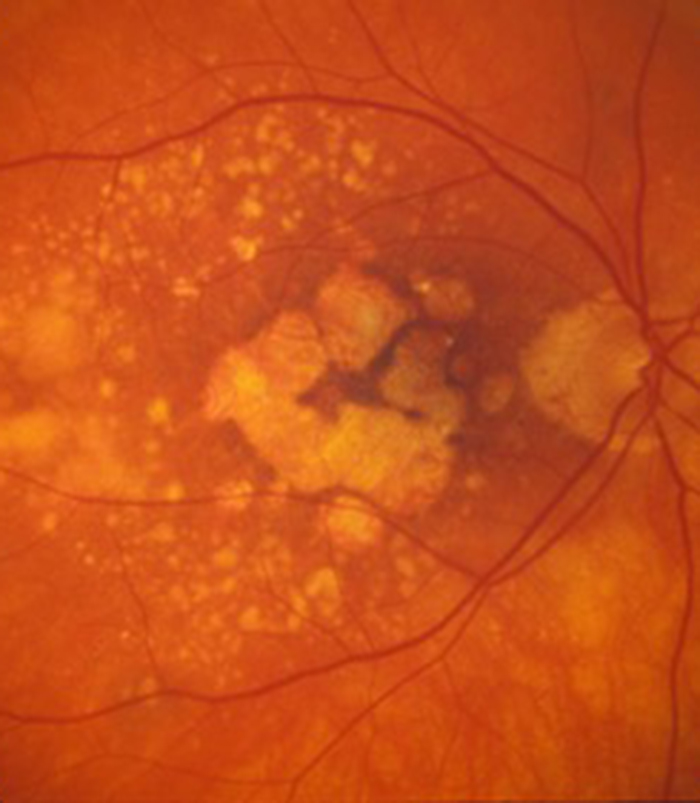
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
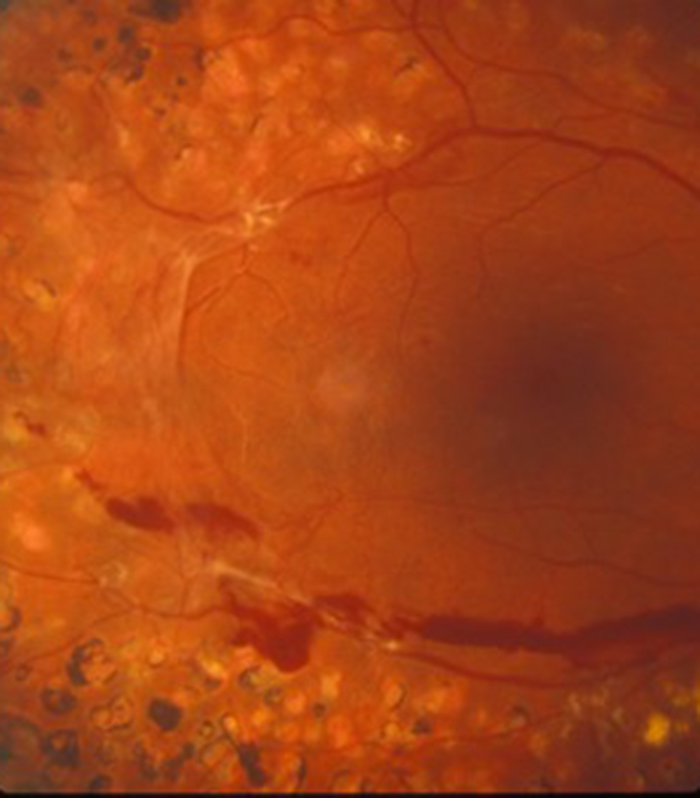
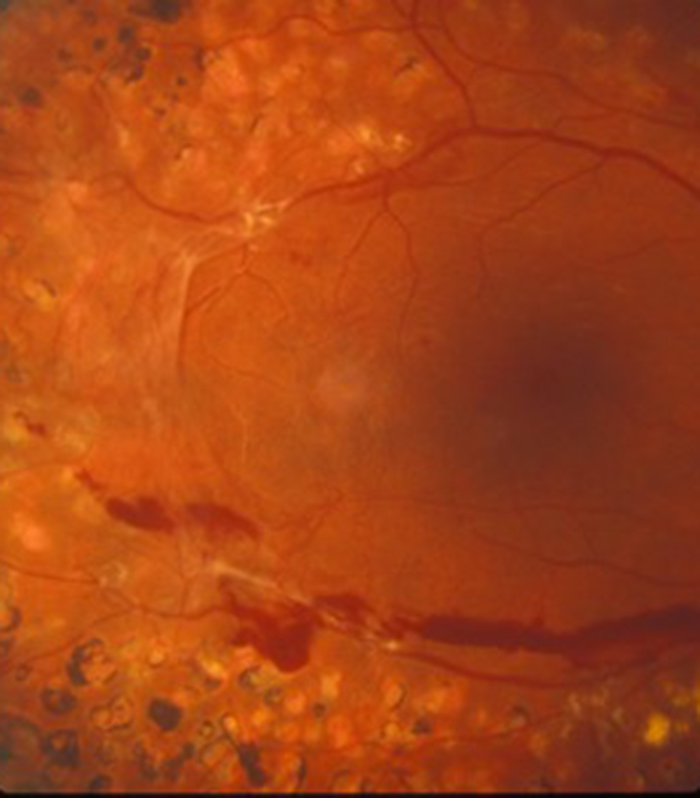
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.


Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

