What is macular degeneration?
The macula is the name given to the centre of the retina (photographic film at the back of the eye). It is responsible for detailed vision (reading, writing, recognising faces) and for colour vision. It is the most sophisticated piece of tissue in the body and works “flat out” from the moment you open your eyes in the morning to the moment you go to sleep. It is responsible for converting the focused image of light striking the retina into electrical impulses that are sent to the brain to give us sight. The cells at the macular that are responsible for changing the light into electricity are called photoreceptors (rods and cones). They work so hard that they need both a very good blood supply called the choroid (to give oxygen and sugar to the cells) and a layer of cells beside them called the Retinal pigment epithelium (RPE) to help them function. The rods and cones need to recycle material in order to function in an efficient manner and the RPE assists in this recycling.
As the macular is working “at full stretch” it is not surprising that with the passage of time it is more prone to the ageing process than other tissues in the body. The light that focuses on the macula and in particular the blue end of the spectrum has high energy and can damage the cells in a variety of ways. The high energy light can produce particles called “free radicals” which damage the cells and the high energy light can also damage the genetic material in the cells called “DNA” that controls the function of the cell.
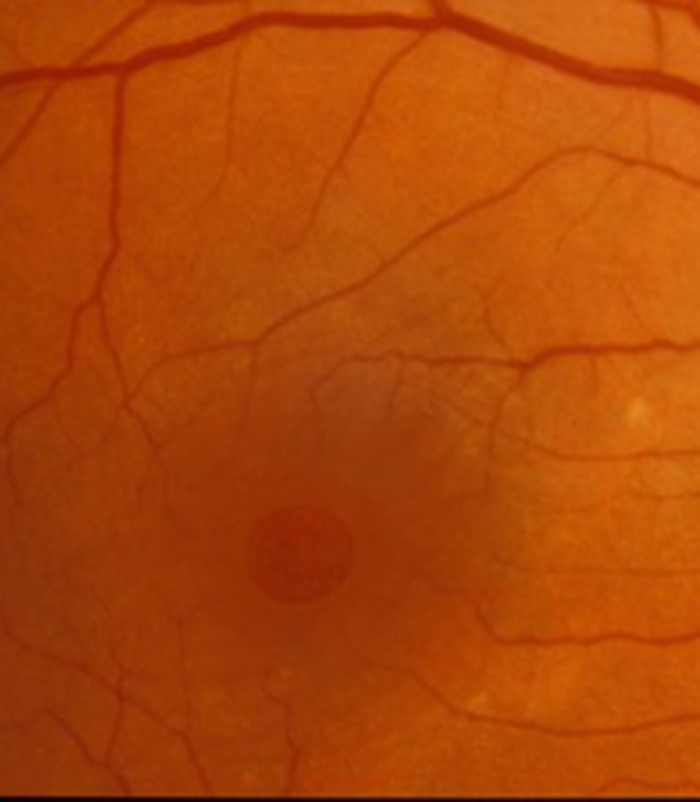
The RPE recycling also becomes less efficient with the passage of time and “waste products” accumulate within the retina called “drusen”
The eye has some defence against this ageing process. Lutein is a pigment that you get from your diet and is present at the macula and helps prevent the high energy blue light from reaching the rods and cones. Anti-oxidant vitamins (such as vitamin C and E) help “mop up” the damaging “free radicals” and this is how vitamin supplements are thought to be beneficial in some patients with macular degeneration. Unfortunately the light damage to the DNA cannot be repaired as the retina (and macula) are part of the central nervous system (part of the brain) and they can only scar and not regenerate or repair easily.
A small number of patients have inherited genes that make them more prone to developing macular degeneration and may develop it at a younger age.
Smoking is a very bad thing for the body for a large number of reasons and this also includes increasing your risk of developing severe macular degeneration.
What are the symptoms of macular degeneration?
Macular degeneration is the most common cause of loss of vision in patients over the age of 55 in the Western World. Patients complain of a blurred patch in the centre of the vision or sometimes distortion of vision (straight lines looking kinked or uneven). It must be emphasised however that it is not a blinding condition and does not lead to complete loss of vision. It only involves the central retina (macula) which is an important but small part of the retina. The side or peripheral retina is unaffected and therefore the side vision or peripheral vision is maintained.
This enables patients to see to navigate around and remain independent. The healthy peripheral retina is also the reason why magnifiers are of benefit to patients with this condition as the image is enlarged onto this. Symptoms usually develop gradually with dry macular degeneration but are of sudden onset with wet macular degeneration (see below).
Patients with mild macular degeneration are often aware that vision is better in good light and that on waking from sleep in the morning there is often a blurred patch in the centre of the vision that gradually fades. When you wake up in the morning and the lids open, the retina has to start work straight away with the rods and cones converting the light into electricity. In early macular degeneration these cells take longer to “get going” and often need more light to function well and this is the reason for developing these symptoms. It can also result in difficulty seeing if you wake up in the night to go to the toilet as the macula again takes time to adjust when the light is switched on. Some patients also find it difficult going from a brightly lit environment such as outside on a sunny day to a poorly lit room in the house as it takes longer to adjust to the new level of lighting. Patients that are either driving or a passenger in a car that passes thought a road with overhanging tree branches also may find it difficult adjusting to the quick sequence of dark and light patches in the road if they have macular degeneration.
Patients with severe macular degeneration and very poor vision can sometimes develop visual hallucinations called Charles Bonnet syndrome. These may take the form of colours or shapes or more detailed hallucinations such as seeing people who are not there. Almost one third of all input to the brain comes from the eyes so if you have severe macular degeneration there is a large amount of your brain that is not stimulated by the eyes so the brain makes up its own images and hence the development of the hallucinations. They usually settle although can be very disconcerting when they first develop. There is no good medical treatment at present for these hallucinations but patients are often reassured when they are told of the diagnosis that there is not a more serious cause for the symptoms.
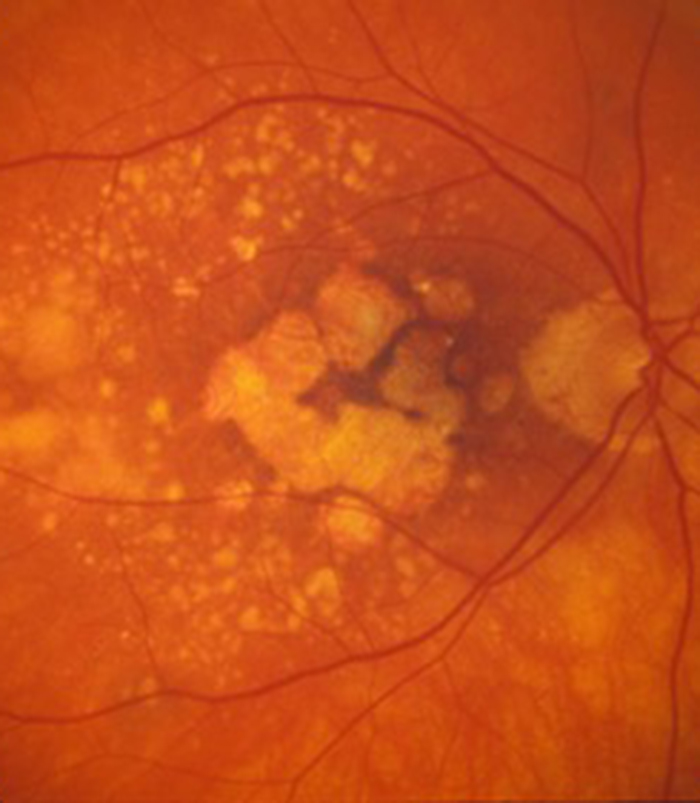
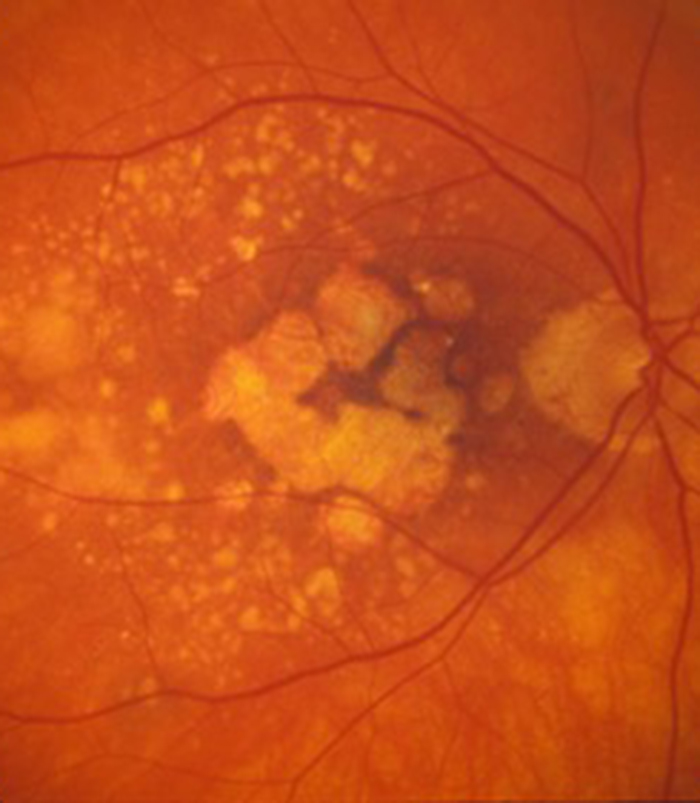
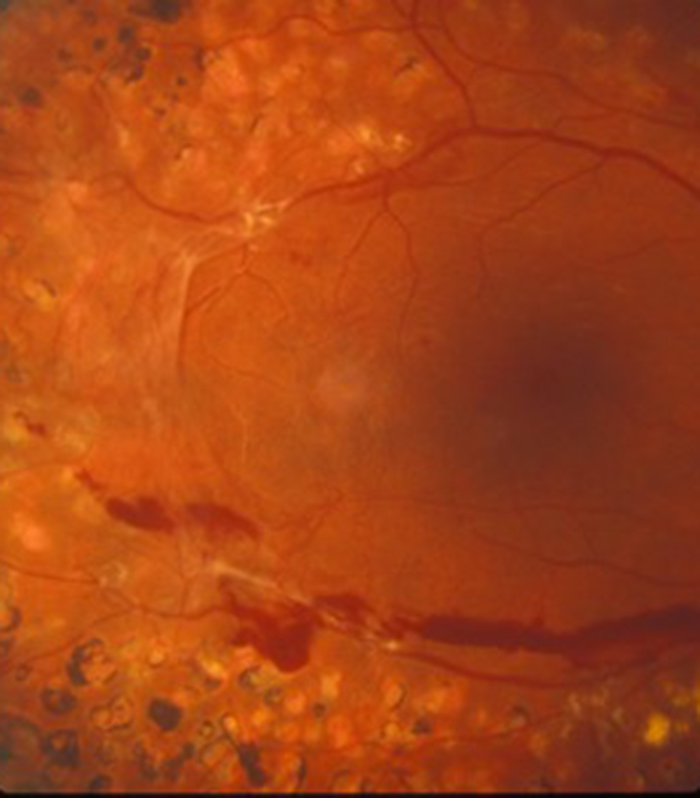
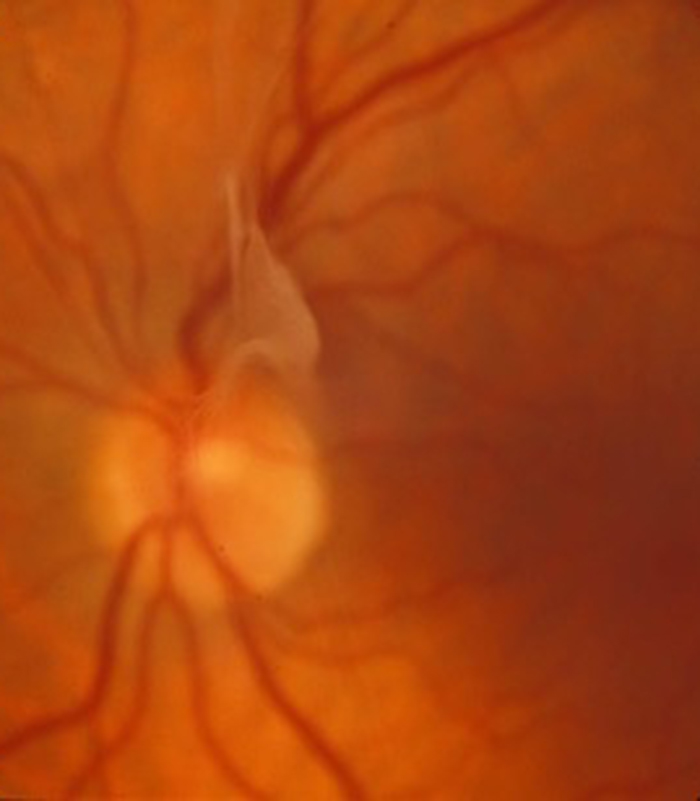
There are two types of macular degeneration, dry and wet. This has nothing to do with dryness of the eye or watering of the eye which related to conditions on the surface of the eye (at the front of the eye). Dry macular degeneration is the gradual “wear and tear” of the macular that occurs with age but wet macular degeneration occurs when abnormal blood vessels develop from under the retina and haemorrhage and leak into the retina.
What is the treatment of wet macular degeneration?
Treatment for wet age-related macular degeneration (AMD) improved significantly from 2006 with the development of the drugs Lucentis (Ranibizumab), Avastin (Bevacizumab) and Eylea (Aflibercept). They are a class of medication called anti-VEGF drugs. Prior to this date the only treatment available for wet AMD were various forms of laser treatment with limited efficacy. The natural course of wet macular degeneration is that the central vision can deteriorate significantly in the first 6 months following the development of the condition with the greatest deterioration within the first few months. The development of anti-VEGF drugs for the first time resulted in a treatment that could improve the vision in a significant minority of patients and prevent the vision from getting worse in most patients.
These types of drug were first developed to treat cancer patients. In order for a cancer to grow it needs a good blood supply to nourish the cancer cells. The body in health produces a chemical called VEGF (vascular endothelial growth factor) that results in new blood vessel formation but VEGF is also produced by tumour cells to help supply blood to the tumour. The drugs are called anti-VEGF drugs as they stop VEGF from working. They are a type of antibody (made from protein) that attaches to the VEGF protein and stops it from working. If there is no functioning VEGF present it impairs the blood supply to the tumour and can help destroy the tumour.
Wet AMD is obviously not a cancer but it is associated with abnormal blood vessels developing from beneath the retina and growing into the retina with the abnormal blood vessels haemorrhaging and leaking causing bruising and water logging of the retina. This can happen suddenly and hence patients with wet AMD can suddenly develop central blurring and distortion of vision. The sooner wet AMD can be treated the better and Eylea, Lucentis and Avastin all reduce the leakage from these abnormal blood vessels. The aim of treatment is to reduce the leakage as quickly as possible and prevent further leakage to minimise the risk of subsequent scar tissue formation. A scarred macular is no longer able to function and results in permanent loss of central vision.
The ideal situation is that treatment is started within 2 weeks of developing symptoms of wet macular degeneration. Sometimes it can be difficult to know when the disease started especially if the other eye is still maintaining good vision. It is easy to loose a large amount of vision in one eye and not notice a problem if the other eye is still functioning well until you happen to cover the good eye and “suddenly” are aware of the poor vision in the other eye.
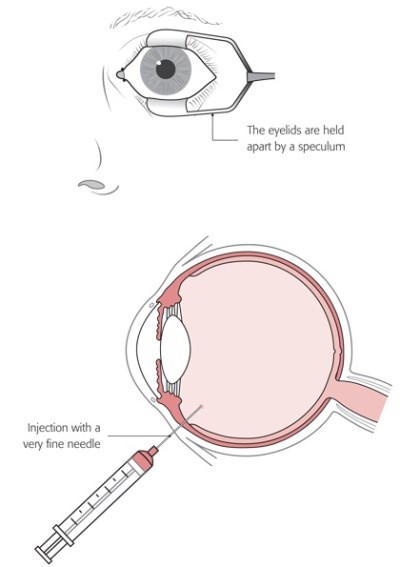
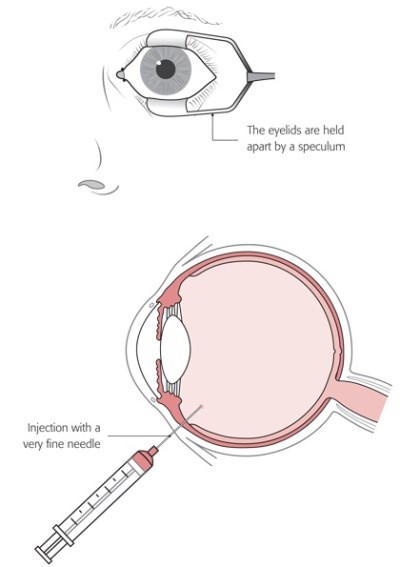
Drops are given to numb the surface of the eye and then a solution of weak iodine is placed on the surface of the eye and the skin around the eye also cleaned with iodine (unless you are allergic to iodine when another cleaning solution is used). This may sound old fashioned but iodine is still the best thing for quickly destroying any bugs (bacteria) that are on or around the eye and therefore minimises the risk of infection.
The face is then covered with a light paper drape with a small hole that allows access to the eye that is having the injection. The drape is held away from the face so that you do not feel claustrophobic. A small instrument called a speculum is placed to keep the lids apart and stop you from blinking so sometimes you are aware of a gentle pressure on the lids that can feel a little strange at first but is not painful. You may be asked to look in a particular direction depending on where the injection is to be given. The injection is over in a second or two and the whole process usually only take a few minutes. After the injection the drape is removed (sometime there is a little pulling on the skin as it is removed) and an antibiotic drop placed on the eye. Some patients at greater risk of infection may be asked to put antibiotic drops into the eye four times a day for 5 days to minimise the risk of infection but most patients do not need to take drops after the injection.
If you do need to put in drops this is performed by first washing your hands then gently pulling the lower lid down and away from the eye and placing a drop in the groove created between the inner aspect of the lower lid and the eye. If you think you have “missed” put another drop in as you cannot “overdose” on these eye drops. There are no other “dos or don’t” after the injection.
Eylea, Lucentis and Avastin usually do require repeated injections in order to maintain the beneficial effect on the vision. They should not be given more frequently than at monthly intervals and most treatments require an initial course of 3 injections or more every month until the vision improves as much as possible then “top up” injections from time to time to try and maintain the improvement in vision or prevent the vision from deteriorating. Many patients have a “treat and extend” regime where injections are continued to be given routinely after the initial course of 3 injections but at every increasing intervals provided the macular remains without leakage on the OCT scan. If leakage is noted then the interval between injections is shortened again. Such a regime would possibly require injections every month for 3 months, then at 6 weeks, then at 8 weeks, then at 10 weeks and so on. A small number of patients only need a few injections to produce a good effect but most require injections from time to time. Unfortunately a small number of patients do not respond to treatment or only partially respond.
There is limited evidence to show a slightly increased risk of heart attacks and strokes with these anti-VEGF treatment but the patients requiring this treatment are usually in the age range where such events occur in any case. The injection treatments are therefore very safe but as a precaution I try and avoid giving injections if someone has recently had a heart attack or stroke (usually within the last 3 months).
What other treatments are needed for macular degeneration?
A good light is vital when reading with a diffuse light over your shoulder. A north facing window will provide excellent light. Any reading material should ideally be with good contrast (black on white) and large print books are of great benefit if you have mild macular degeneration. There are a variety of low visual aids which are mainly based on the principle of magnification of the image onto the healthy peripheral retina (away from the macula).
The minimum amount of magnification that is needed to help reading is required as the greater the amount of magnification the smaller the number of words or letter you see at one time and this makes it more difficult to see the “flow of words”. The amount of magnification needed however depends on the severity of the macular degeneration with greater magnification needed with more severe disease. Some optometrists (opticians) specialise in low visual aids and sometime there are special “drop in” centres with a large number of low visual aids to try. The low visual aids range from strong reading glasses, through a large range of hand held and stand magnifiers (some with built in illumination) to close circuit television devices when the print to be viewed is magnified onto a computer screen. Most low visual aids are to assist with reading but some telescopic devices are also beneficial for distance vision (such as seeing the number of a bus in the distance).
Many patients find great benefit in the use of Kindle’s and iPads’. There are now excellent devices with good contrast and large screens and the font can be magnified easily with your fingers to the correct amount for your particular needs. Don’t forget that if you are using a computer it is easy to enlarge the font size of web pages. If you are a PC user hold the Control (Ctl) key on the bottom left of your keyboard then use the + or – keys at the top right of your keyboard to enlarge or reduce font size. If you are a Mac user hold the Command (cmd) key on the bottom left of your keyboard then use the + or – key top right to change font size.
There are also many other things to help people with visual impairment such as talking books, and various modifications to the house to help you remain independent. It is important to ensure that your local social services are aware of your visual impairment so that you obtain all the benefits available to you and if your sight is sufficiently impaired you should be registered as partially sighted or severely sight impaired. You local eye doctor should perform this for you.
Some eye clinics have an eye clinic liaison officer (ECLO) to inform you about the various supporting agencies that are available to assist in helping patients with a visual disability.
What about vitamins and macular degeneration?
If you are a smoker then the single most important thing that you can do is stop smoking. Patients with mild macular degeneration should have a heathy balanced diet with plently of fresh fruit and dark green leaved vegetables. If you have more significant macular degeneration then you should take a vitamin supplement with the AREDS 2 formula containing Vitamin C, Vitamin E, Lutein, Zeaxanthin, Zinc and Copper. Patients who should be taking the AREDS 2 formula are those patients with wet macular degeneration in one eye and dry changes in the fellow eye and those patients with medium to high risk characteristics of converting from dry to wet degeneration. This depends on the appearance of the macular and you can only get guidance on this from your optometrist or eye doctor. The yellow drusen that is found in dry macular change can have different appearances. Small “hard” looking drusen are at lower risk of progressing to wet macular degeneration than large “soft” looking drusen. It is this latter group of patients who should be taking the AREDS 2 formula. The optometrist may be able to tell you what type of drusen and advise on vitamin supplements.
Following on
Please click on the video below to see a talk I gave on macular degeneration at the “Top Doctors” seminar organised by the Macular Society and Royal College of Ophthalmologists.
Problems we can help with
I will explain with the aid of video clips the various eye problems I treat. This includes cataract surgery, refractive lens exchange in patients over 50 and medical and surgical treatments of all retinal and macular problems.
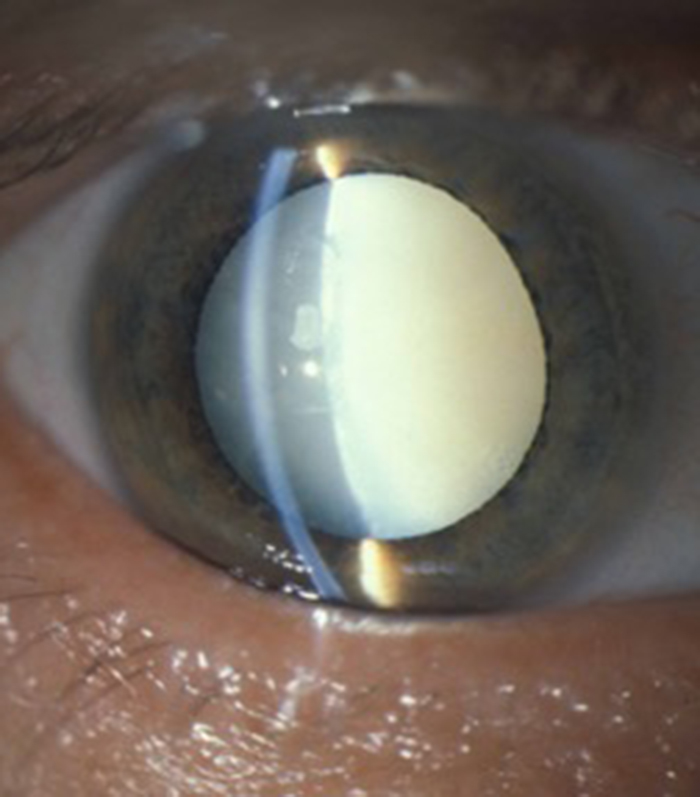
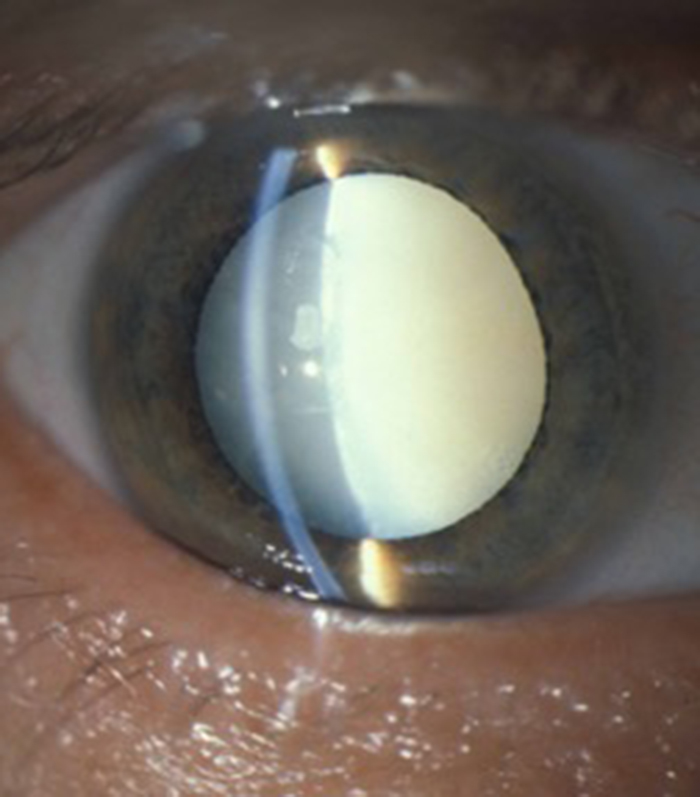
Cataract
I provides advanced micro-incision cataract surgery and will advise on the appropriate intra-ocular lens for your particular needs. This includes toric lenses to correct astigmatism and extended range of vision multifocal lenses to reduce spectacle dependance.
Macular Degeneration
Patients with wet (neovascular) age-related macular degeneration can benefit from prompt injection treatments with various anti-VEGF agents. The first injection can usually be performed on the day of consultation as as "see and treat service".
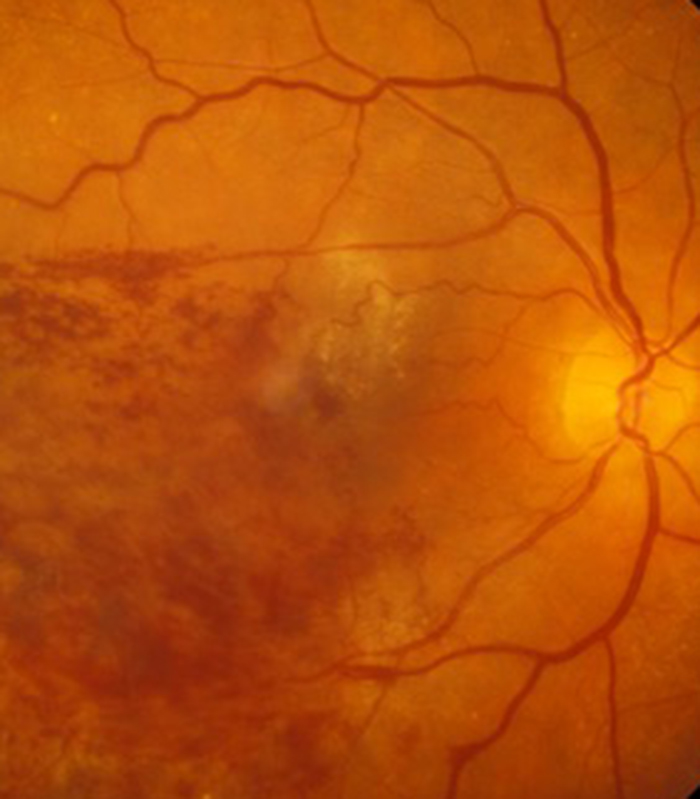
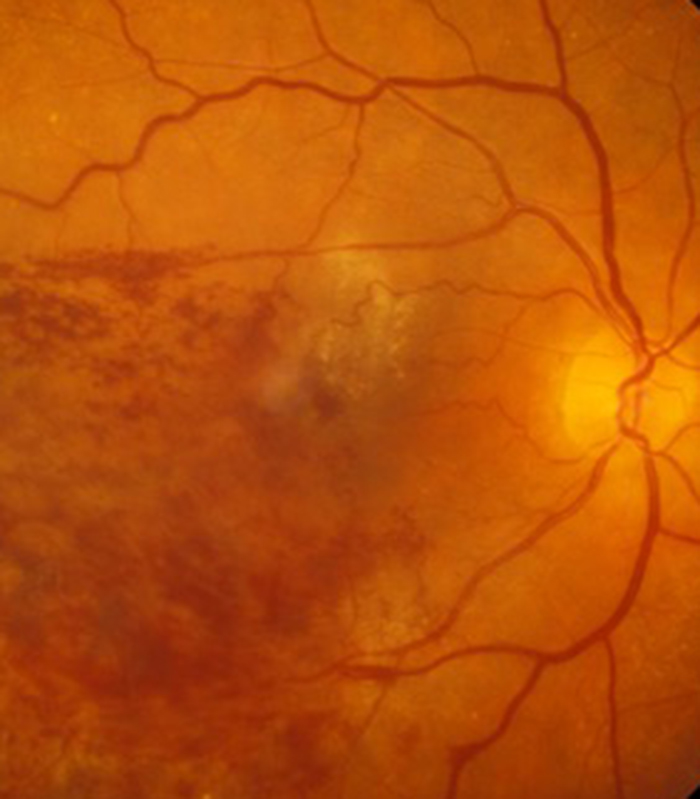
Retinal Vein Occlusion
Blockage to the veins of the retina can produce significant visual disturbance and may require injection treatments with anti-VEGF agents or steroids at Exeter Eye. More severe cases may require laser or surgery at the West of England Eye Unit under Mr Simcock's care..
Diabetic Eye Disease
Diabetes is becoming increasingly common and can cause significant visual loss. If detected at an early stage vision can be maintained using injection treatments with anti-VEGF agents or steroids. More serious cases may require laser or surgery at the West of England Eye Unit.
Macular Hole
Mr Simcock has pioneered macular hole surgery in the UK and performs a technique which includes lens removal to prevent patients returning for cataract surgery. The technique also benefits from no or limited (2 day) face down posturing to allow hole closure in most macular holes.


Epiretinal Membrane
Scar tissue on the surface of the macular (central retina) causes blurring and distortion of vision. Surgical removal of scar tissue with vitrectomy can be performed if sufficiently troubled. Most patients notice a significant improvement in vision and reduced distortion with this surgery..
Floaters
Patients troubled by floaters in their vision not improving over a period of at least 6 months may benefit from vitrectomy surgery to remove the floaters. Patient selection is important and depends on age (usually over 50) and the state of the jelly (vitreous) in the main eye cavity.

